Understanding Parkinson’s Disease:
A Beginner's Guide
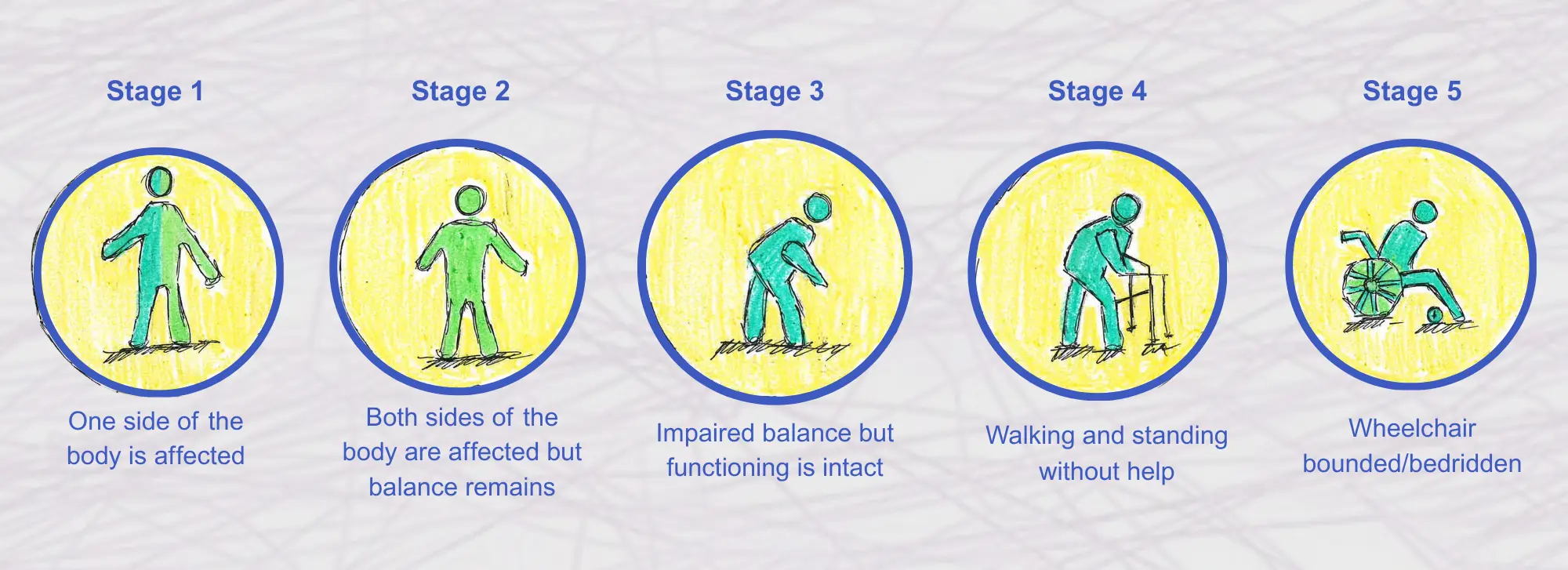
Stages of Parkinson’s Disease
Parkinson’s Disease progresses gradually, with the severity of symptoms increasing over time. Understanding the stages of Parkinson’s can help patients, caregivers, and healthcare professionals plan for the future and adjust treatment strategies.
Stage 1: Mild Symptoms
- Characteristics: Symptoms are modest, usually affecting only one side of the body (unilateral). Tremors or other movement- related symptoms may be present but do not significantly interfere with daily activities.
- Impact on Daily Life: Individuals in Stage 1 can continue with most of their usual activities with minimal or no assistance. They may notice a slight change in posture, walking, or facial expressions.
- Example: Mrs. Gupta, a 62-year-old woman, noticed a slight tremor in her left hand. She continued with her daily chores and activities, only occasionally feeling discomfort.
Stage 2: Bilateral Symptoms
- Characteristics: Symptoms worsen and start affecting both sides of the body (bilateral). Problems with walking and posture become more apparent.
- Impact on Daily Life: Daily tasks may take longer, and there may be noticeable changes in the way a person walks (gait). Some individuals may begin to experience stiffness in the muscles.
- Example: Mr. Singh, a 68-year-old man, began to experience tremors in both hands. He also noticed that his movements had slowed down and he felt stiffer in the mornings.
Stage 3: Mid-Stage
- Characteristics: This stage is characterized by significant slowing of movement (bradykinesia) and balance problems. Falls become more common.
- Impact on Daily Life: Daily activities such as eating, dressing, and bathing may require assistance. Individuals may find it challenging to maintain their balance, increasing the risk of falls.
- Example: Mrs. Patel, a 70-year-old woman, found it increasingly difficult to button her shirt and tie her shoes. She also noticed that she had to be more cautious while walking to avoid tripping.
Stage 4: Severe Symptoms
- Characteristics: Symptoms are severe and limiting. Movement is greatly reduced, and assistance is needed for most daily activities.
- Impact on Daily Life: At this advanced stage, individuals may require a walker or wheelchair to move around. They may need help with personal care, and their ability to live independently is significantly reduced.
- Example: Mr. Rao, a 75-year-old man, relied on his wife and a caregiver for most of his daily activities. He used a walker to move around the house and needed help with dressing and eating.
Stage 5: Advanced Stage
- Characteristics: Patients with stage 5 may be bedridden or in a wheelchair and present with severe motor and non-motor symptoms, including dementia.
- Impact on Daily Life: Individuals require around-the-clock care. They may struggle with basic functions such as swallowing and communicating. Cognitive symptoms, such as confusion and dementia, may also be prominent.
- Example: Mrs. Das, an 80-year-old woman, was bedridden and required full-time care. She experienced severe cognitive decline and had difficulty recognizing family members.

Mr. Verma, a retired teacher from Delhi, was diagnosed with Parkinson’s Disease at the age of 60. Initially, his symptoms were mild, with a slight tremor in his right hand. As the years passed, his symptoms gradually worsened. By the age of 70, Mr. Verma had reached Stage 4, where he needed assistance with most of his daily activities. His wife became his primary caregiver, helping him with tasks such as dressing and eating. Despite the challenges, Mr. Verma remained mentally sharp, enjoying reading and spending time with his grandchildren. However, by the age of 75, his symptoms had progressed to Stage 5, and he required full-time care. Understanding the stages of Parkinson’s helped Mr. Verma and his family prepare for the changes and plan for his care needs.
Disclaimer: This example is just for understanding purposesCauses and Risk Factors
Research indicates that a mix of environmental and genetic factors contribute to the development of Parkinson’s disease, even though its precise causes is still unknown.
Genetic Factors
Familial Parkinson’s Disease: In about 10-15% of cases, Parkinson’s Disease is familial, meaning it runs in families. Certain gene mutations, such as those in the LRRK2, SNCA, PRKN, PARK2, PARK7, and PINK1 GBA and DJ-1 genes, etc. have been identified as contributors to hereditary Parkinson’s. These cases tend to present earlier in life.
Non-Genetic Factors
Sporadic Parkinson’s Disease: Most Parkinson’s disease cases are sporadic, which means they happen to people who don’t have a family history of the condition. Although the exact cause is unknown, researchers believe that a combination of environmental factors and genetic susceptibility triggers the disease.
Toxin Exposure: An elevated risk of Parkinson’s disease has been linked to exposure to specific environmental pollutants, including metals, pesticides, and herbicides. Using well water has also been linked to an increased incidence of Parkinson’s disease (PD), potentially as a result of pesticide exposure. For example, greater incidence rates have been associated with farming and rural living, both of which may expose people to toxic substances.

Drugs: Certain drugs including NSAIDs, thiazolidinediones, oral contraceptives, calcium channel blockers, typical & atypical antipsychotic drugs, dopamine deplete drugs, hormone replacement therapy, acetaminophen/paracetamol, beta-blockers, statin are linked with increased risk of Parkinson’s disease.
Head Trauma: A higher risk of Parkinson’s disease has been linked to repeated head traumas, such as those received in collisions or contact sports. Head trauma may contribute to the development of the disease by causing inflammation and neurodegeneration in the brain.
Mr. Naik, a 65-year-old farmer from Maharashtra, had been exposed to pesticides for decades while working in his fields. In his early 60s, he began to notice a tremor in his left hand and stiffness in his limbs. He was diagnosed with Parkinson’s disease by a neurologist, and it was speculated that his prolonged exposure to pesticides may have played a role in the onset of the illness. Mr. Naik’s case highlights the potential impact of environmental factors on the risk of developing Parkinson’s Disease, particularly in populations with high exposure to toxins.
Disclaimer: This example is just for understanding purposes
Diagnosis of Parkinson’s Disease
A neurological examination, medical history, and the exclusion of other health conditions that could be causing the same symptoms are all part of the diagnosis process for Parkinson’s disease. Although there isn’t a single, conclusive test for Parkinson’s disease, a number of methods are employed to get a diagnosis.
Medical History and Examination
- Patient History: A thorough history of the patient’s symptoms, including their onset and development is taken by the neurologist. The doctor also inquires about any family history of PD or related conditions.
- Neurological Examination: The neurologist will conduct a detailed examination to evaluate the patient’s motor skills, reflexes, muscle tone, balance, and coordination. The presence of tremors, bradykinesia, rigidity, and postural instability will be evaluated.
Imaging Tests
- MRI and CT scans: Computed tomography (CT) and magnetic resonance imaging (MRI) scans can help rule out other disorders like strokes or brain tumors that may cause similar symptoms, but they cannot be used to directly diagnose Parkinson’s disease.
- DaTscan: A DaTscan is an imaging test that can help foresee the dopamine transporter in the brain. It is used to distinguish Parkinson’s disease from other movement disorders, including drug- induced Parkinsonism and tremors. However, it is not a definitive test for Parkinson’s and is typically used in conjunction with clinical evaluation.
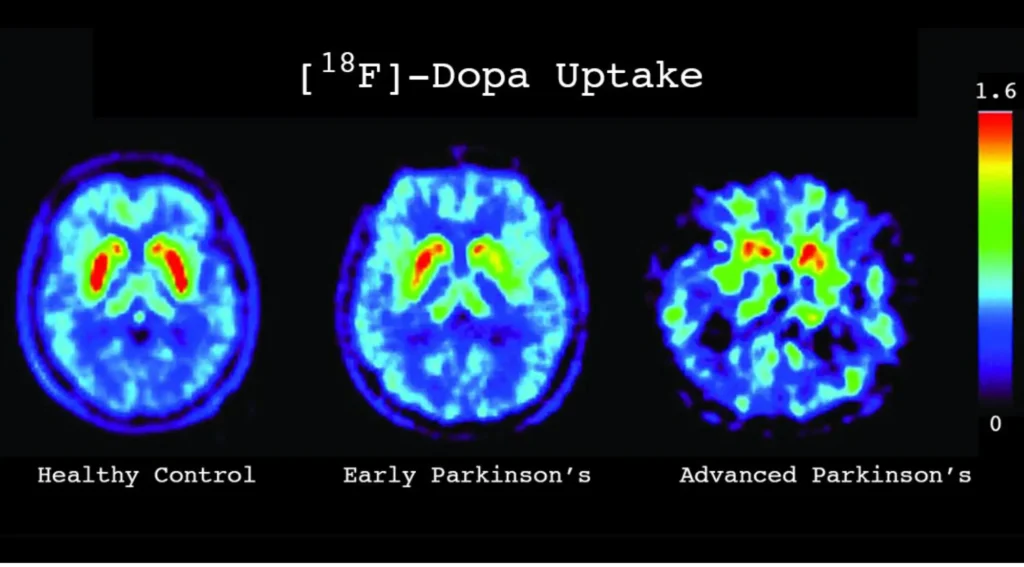
Dopaminergic uptake in healthy control and Parkinson’s disease. Image adapted from the webpage of Davis Phinney Foundation.
Representative axial brain PET images showing [^18F]-Dopa uptake in the striatum. Warmer colors (red–yellow) indicate higher dopaminergic activity, while cooler colors (green–blue) indicate reduced uptake.
– Left: Healthy control demonstrating symmetric, high tracer uptake in the bilateral striatum.
– Middle: Early Parkinson’s disease showing reduced and asymmetric uptake, typically beginning in the posterior putamen.
– Right: Advanced Parkinson’s disease with marked bilateral reduction in striatal uptake, reflecting progressive dopaminergic neuronal loss.
Color scale represents relative tracer uptake intensity (0–1.6).
Trial of Parkinson’s disease Medications
Levodopa Response Test: One way to support a diagnosis of PD is to observe the patient’s response to Levodopa, a medication that increases dopamine levels in the brain. Levodopa may indicate Parkinson’s disease if the patient’s symptoms considerably improve after taking it.
Differential Diagnosis
A list of possible conditions that share the same symptoms as described by the patient:
- Multiple System Atrophy (MSA): It is an uncommon neurological condition that combines autonomic dysfunction, including high blood pressure, along with symptoms resembling Parkinson’s disease.
- Progressive Supranuclear Palsy (PSP): A condition that can cause symptoms resembling Parkinson’s disease, like bradykinesia and stiffness, but is distinguished by difficulties with eye movements and balance.
- Corticobasal Degeneration (CBD): Another rare condition that causes asymmetric Parkinsonian symptoms but is characterized by more severe cognitive and motor symptoms.
- Drug-induced Parkinsonism (DIP): A condition that shows asymmetrical parkinsonism and tremor at rest, making it difficult to differentiate from PD.
Mrs. Reddy, a 63-year-old woman from Hyderabad, began experiencing a tremor in her right hand and stiffness in her neck. Her symptoms gradually worsened, and she noticed that her movements had slowed down significantly. Concerned about her symptoms, Mrs. Reddy consulted her family doctor, who referred her to a neurologist. The neurologist conducted a detailed examination and suggested an MRI to rule out other conditions. After considering her medical history, symptoms, and a positive response to Levodopa, Mrs. Reddy was diagnosed with Parkinson’s Disease. The diagnosis allowed her to start treatment early, helping to manage her symptoms and maintain her quality of life.
Disclaimer: This example is just for understanding purposes