Understanding Parkinson’s Disease:
A Beginner's Guide
Treatment Options for Parkinson’s Disease
Although Parkinson’s disease cannot be cured, there are several therapeutic options that can help control symptoms and enhance quality of life. Usually, supportive therapy, surgery, and medication are used in combination for treatment.
Medications
Most medications aim to replenish or mimic dopamine, the neurotransmitter that is deficient in patients with Parkinson’s.
- Levodopa-Carbidopa: The most effective medication for managing the symptoms of Parkinson’s disease is levodopa. In the brain, it is transformed into dopamine, which eases motor problems. Levodopa and carbidopa work together to reduce adverse effects including nausea by preventing the drug’s early conversion to dopamine outside the brain.
- Dopamine Agonists: These drugs are frequently used in the early stages of Parkinson’s disease or in combination with levodopa because they imitate the effects of dopamine in the brain. Examples include Ropinirole, Pramipexole, and Rotigotine. Dopamine agonists can be associated with side effects like drowsiness and impulsive behaviors.
- Monoamine oxidase B (MAO-B) inhibitors: MAO-B Inhibitors like Rasagiline and Selegiline, block dopamine disintegration in the brain, elongating its effects. They are often used in the early stages or as an supplement to Levodopa.
- Catechol-O-methyltransferase (COMT) inhibitors: COMT Inhibitors like Tolcapone and Entacapone elongate the effect of Levodopa by blocking the dopamine-breaking enzyme. These are typically used in patients experiencing “wearing-off” effects with Levodopa.
- Amantadine: Amantadine, an antiviral drug, helps lessen dyskinesias (involuntary movements) associated with prolonged Levodopa use. It may also have some benefit in controlling tremors.
- Anticholinergics: Anticholinergic medications including Benztropine, Trihexyphenidyl HCl are used to alleviate the tremor by blocking
acetylcholine in the brain, a chemical that modulates movement. They are often used in younger people either as a monotherapy or combination therapy.
Invasive/Non-invasive treatments
For patients who experience significant motor fluctuations or who don’t react well to medicine, advanced invasive treatment strategies may be considered.
- Deep Brain Stimulation (DBS): The most commonly used surgical treatment for Parkinson’s Disease is DBS. It requires implanting electrodes in particular brain regions, like the globus pallidus or subthalamic nucleus, that are linked to a pulse generator that is positioned in the chest. To minimize symptoms including bradykinesia, stiffness, and tremors, the device sends electrical impulses to the brain. DBS is especially helpful for people who have dyskinesias or motor irregularities that are difficult to treat with medicine alone.
- Lesioning Procedures: In some cases, surgical procedures that create small lesions in specific brain areas, such as pallidotomy or thalamotomy, may be performed to control symptoms. However, these procedures are less commonly used today due to the availability of DBS.
- Continuous dopaminergic stimulation therapy: Apomorphine pump is a light weight pump used to treat motor symptoms in Parkinson’s disease by stimulating dopamine production.


It is one of the less-invasive and effective treatment options for those patients with PD when oral medications are slow/inadequate to act or patients can’t undergo DBS.
- Duodopa pump: For severe Parkinson’s disease, DuoDopa is a gel that combines levodopa and carbidopa and is injected straight into the small intestine via a surgically inserted tube. It can lessen off time and assist keep levodopa’s plasma concentration steady.
- Focused ultrasound therapy: Focused ultrasound therapy (FUS) is a non-invasive procedure that uses ultrasound beams to alleviate symptoms of Parkinson’s disease by disrupting circuits linked to tremor.
Supportive Therapies
Aside from drugs and surgery, several therapies can help control Parkinson’s disease symptoms and enhance quality of life.
- Physical Therapy: Improving strength, balance, and mobility are the main goals of physical therapy. Exercises that improve posture, flexibility, and coordination can help patients maintain mobility and lower their risk of falling.
- Occupational Therapy: Occupational therapy assists patients in adapting to the physical challenges of Parkinson’s Disease. Therapists help patients become better at doing everyday tasks including eating, writing, and dressing. They may also recommend assistive devices to enhance independence.
- Speech Therapy: Speech and swallowing issues are common in Parkinson’s disease patients. Speech therapists can help patients improve their communication skills through exercises that strengthen the muscles used in speech. Additionally, they can offer methods for controlling swallowing issues and lowering the risk of aspiration.
- Dietary Management: Patients with Parkinson’s disease can benefit from a balanced diet full of fruits, vegetables, healthy grains, and lean meats. Some patients may benefit from a diet high in fiber to manage constipation, a common non-motor symptom. Additionally, patients on Levodopa may need to adjust their protein intake, as high- protein meals can interfere with the absorption of the medication.

Mr. Iyer, a 70-year-old man from Chennai, was diagnosed with Parkinson’s Disease five years ago. His neurologist prescribed Levodopa-Carbidopa, which effectively controlled his symptoms for the first few years. As his disease progressed, Mr. Iyer began experiencing “wearing-off” periods, where the medication’s effects would diminish before the next dose was due. His neurologist added a COMT inhibitor to his regimen, which helped prolong the effect of Levodopa.
In addition to medication, Mr. Iyer attended regular physical therapy sessions, which helped him maintain his balance and reduce the risk of falls. He also worked with an occupational therapist to modify his home environment and make daily tasks easier. When Mr. Iyer started having difficulty speaking, he began speech therapy to improve his communication skills. By combining medication with supportive therapies, Mr. Iyer was able to manage his symptoms and maintain his quality of life.
Disclaimer: This example is just for understanding purposesRole of Gut Microbiota in Parkinson’s Disease
- According to research, the gut-brain axis—a biochemical exchange between the central nervous system and the gastrointestinal tract—is how what occurs in the gut affects the brain.
- Although research on Parkinson’s disease and the microbiome is still in its early stages, studies suggest that gut microbiota, diet, and lifestyle may influence the progression and symptoms of PD.
Foods That Support Gut Microbiota and May Help Slow Parkinson’s Progression
- High-Fiber and Plant-Based Foods (Mediterranean-Style Diet)
- Fiber-rich foods fuel beneficial gut bacteria, producing short-chain fatty acids that reduce inflammation and support brain health.
- Examples: Whole grains (oats, quinoa, brown rice), Fruits (grapes, cranberries, bananas), Vegetables (artichokes, onions, garlic, chicory root), Legumes (beans, lentils), Nuts and seeds.
- Healthy Fats
- Supports brain and heart function while reducing inflammation.
- Examples: Extra virgin olive oil, Nuts (almonds, walnuts), Seeds (flaxseeds, chia seeds)
- Prebiotic Foods
- These promote the growth of beneficial gut bacteria.
- Examples: Bananas, onions, garlic, Chicory root, beans, grapes, and cranberries.
- Probiotics
- Live beneficial bacteria (found in fermented foods like yogurt).
- Protein Timing for Parkinson’s Medications
- A protein-redistribution diet (consuming most protein during the last meal of the day).
- High-Protein Foods to Monitor: Meat, fish, eggs, dairy, Nuts, beans.
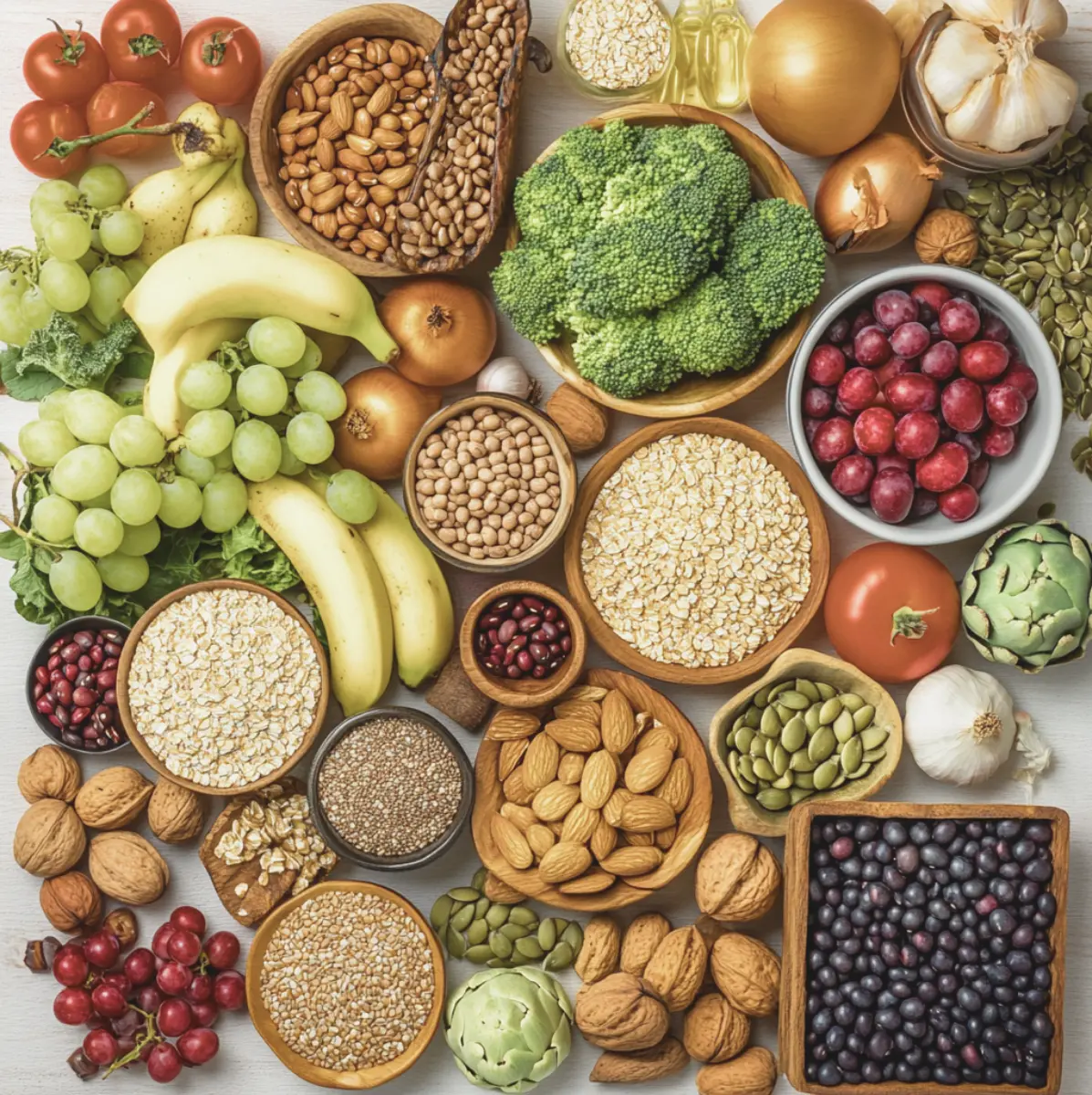
This diet-focused approach may help support gut health, reduce inflammation, and improve PD symptoms.
Disclaimer: Based on observational studies, gut microbiota may play a role in Parkinson’s disease; however, no randomized controlled trials (RCTs) have been conducted to date, and the causal relationship remains under investigation. Therefore, the dietary recommendations provided here should be considered as soft guidelines rather than definitive medical advice.

Living with Parkinson’s Disease
Living with Parkinson’s Disease is extremely challenging, however; with the right support and treatment management strategies, patients can lead fulfilling lives. Here are some tips and strategies for managing the disease:
Daily Living Tips
- Stay Active: Regular exercise is crucial for maintaining mobility and balance. Activities like walking, swimming, and tai chi can help enhance flexibility, strength, and coordination. Exercise also has mood-boosting benefits, which can help combat depression and anxiety.
- Adopt a Healthy Diet: A well- balanced diet can support overall health and help manage symptoms like constipation. Staying hydrated and eating a variety of nutrient-rich foods can also enhance energy levels and support brain health.
- Create a Safe Home Environment: Making small adjustments to the home can reduce the risk of falls and make daily tasks easier. Installing grab bars in the bathroom, using non-slip mats, and keeping pathways clear of clutter are simple ways to create a safer living space.

- Stay Connected: Social support is essential for mental and emotional well-being. Staying connected with family, friends, and support groups can provide a sense of community and reduce feelings of isolation.
Emotional and Mental Health
- Coping with Depression and Anxiety: Many people with Parkinson’s Disease experience depression and anxiety. If these symptoms arise, it’s important to talk to a healthcare provider, as they can recommend treatments such as medication, counseling, or cognitive-behavioral therapy (CBT).
- Mindfulness and Relaxation Techniques: Practices like mindfulness meditation, deep breathing exercises, and yoga can help reduce stress and improve mental well-being. These techniques can also enhance focus and help manage symptoms like tremors and muscle rigidity.
- Seek Support: Joining a support group can provide valuable encouragement and advice. Sharing experiences with others who understand the challenges of Parkinson’s disease can be incredibly empowering.
Caregiver Support
- Understanding the Role of a Caregiver: Caregivers play a vital role in the lives of people with PD. They provide physical and emotional support, assist with daily tasks, and help manage medical appointments and treatments. Caregivers should be prepared for the progressive nature of the disease and the increasing care needs that arise over time.
- Self-Care for Caregivers: Caregiving can be physically and emotionally demanding. It’s important for caregivers to take time for themselves, seek respite care when needed, and connect with support groups for caregivers. Prioritizing self-care helps prevent burnout and ensures that caregivers can continue to provide the best possible care.

Planning for the Future
- Advance Directives: As Parkinson’s Disease progresses, it may become difficult for patients to make decisions about their care. Having advance directives in place, such as a living will and durable power of attorney for healthcare, ensures that a patient’s wishes are respected.
- Financial Planning: PD can lead to increased medical expenses and long-term care needs. Early financial planning, including exploring options for health insurance and government assistance programs, can help ease the financial burden.
Mrs. Rao, a 65-year-old woman from Bangalore, was diagnosed with Parkinson’s Disease three years ago. She noticed that her movements had slowed down and she had difficulty maintaining her balance. After consulting with her neurologist, Mrs. Rao began taking Levodopa-Carbidopa to manage her symptoms. In addition to medication, she started attending a local Parkinson’s support group, where she met others who were also living with the disease. The group provided her with valuable tips on managing symptoms and staying active. Mrs. Rao also worked with a physical therapist who developed a personalized exercise plan to improve her strength and balance. By staying proactive and seeking support, Mrs. Rao has been able to manage her symptoms and maintain a positive outlook on life.
Disclaimer: This example is just for understanding purposes